Pelvic Health, Reimagined.
Restoring function, rebuilding confidence.
We’re here to help you get back to the life you deserve.
Pelvic pain, incontinence, discomfort with intimacy—these aren’t just “part of life.” At Prairie Pelvic Health, we help you understand what’s happening in your body and work with you to restore comfort, confidence, and control.
What sets us apart
Dedicated to Pelvic Health
Work with therapists who have spent their careers helping those with pelvic issues get back to the life they want!
Finding the "Why"
We are committed to finding the underlying causes of your symptoms so you can find lasting relief.
Full-length Sessions
Hour-long and one-on-one with a skilled pelvic health physiotherapist.
Meet our physiotherapists

Juliet Sarjeant
With 20 years of experience, Juliet helps people reduce pain, move better, and feel confident in their recovery.

Lindsey Tasker Cole
With 13 years of experience, Lindsey specializes in pelvic health, pregnancy and postpartum care, and sports injury rehab.

Danielle Bararuk
Danielle is the newest member of our team ! We are excited to have her at our clinic. Danielle is now accepting new clients!
I’ve seen thousands of people come through these doors unsure, overwhelmed, and in pain—and I’ve seen them leave with knowledge, relief, and hope. That’s why I love this work.
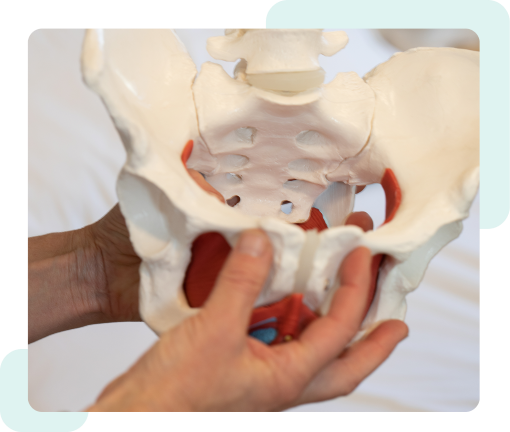
What is pelvic health physiotherapy?
Pelvic health physiotherapy focuses on the muscles, nerves, and tissues in and around your pelvis. Whether you’re dealing with pelvic pain, incontinence, prolapse, or recovering after birth, this type of physiotherapy can help you feel stronger, more comfortable, and more in control of your body.
Why is pelvic health so important?
Your pelvic floor muscles do a lot of behind-the-scenes work to support your daily life. They help control your bladder and bowels, contribute to sexual health, support your internal organs, and stabilize your spine and core. When these muscles aren’t functioning properly, it can affect everything from how you move to how you feel in your own body. That’s why pelvic health isn’t just about one part of you, it’s about your overall well-being.
What does a pelvic health physiotherapist do?
Pelvic health physiotherapists are specially trained to assess and treat conditions related to the pelvic floor muscles, joints, and surrounding tissues. We look at the big picture—your posture, movement, habits, and overall muscle function—and we also have the tools to perform internal examinations when needed to better understand what’s going on beneath the surface. From tailored exercises and hands-on therapy to education and self-management tools, we create a personalized plan to help you feel better and get back to what you love.
What conditions do you treat?
We treat a wide range of pelvic health concerns for people of all genders and life stages. Some of the most common include:
- Urinary incontinence (leaking with movement or urgency)
- Pelvic organ prolapse (feeling pressure or heaviness)
- Pelvic pain (chronic or acute, including during sex or exercise)
- Pregnancy and postpartum recovery (preparing for or healing from birth)
- Men’s pelvic health (including pain, incontinence, and sexual function)
- Transgender pelvic health (support during and after transition-related care)
We also offer pessary fittings and dry needling. Visit the What We Treat section to learn more about each area of care.
What should I expect during my first visit?
We begin with a conversation. Your first appointment is a chance to share your story and for us to understand your goals, history, and symptoms. We’ll assess your posture, movement, and muscle function—and, with your consent, we may recommend an internal exam to help us get a clearer picture of what’s happening. Everything we do is grounded in comfort, respect, and collaboration. You’ll leave with a better understanding of your pelvic health and a personalized treatment plan to guide your care.
What we hear…
“I feel like my body has betrayed me.”
Living with pelvic pain or dysfunction can make everyday activities feel impossible and leave you wondering if you’ll ever feel normal again.


“I used to love being intimate with my partner.”
Pain during intercourse isn’t something you should have to accept or endure silently.
“I feel isolated in my experience.”
You’re not alone—millions of people experience pelvic health issues, but most don’t talk about them.
